Keratoplasty
Vision Outcomes Following Keratoplasty for Keratoconus: Challenges and Considerations
Challenges in Vision Improvement:
1. Persistent Visual Limitations:
Despite undergoing keratoplasty, many keratoconus patients may experience persistent visual limitations due to factors such as irregular astigmatism, corneal haze, and graft-host interface irregularities.
2. Risk of Rejection:
Keratoplasty carries a risk of graft rejection, particularly in keratoconus patients with a compromised ocular surface. Rejection episodes can lead to graft failure and subsequent vision deterioration, necessitating close monitoring and long-term immunosuppressive therapy.
3. Suture-Related Complications:
The use of multiple sutures in traditional keratoplasty techniques poses a risk of suture-related complications, including induced astigmatism, suture abscesses, and vascularization. These complications can impact visual outcomes and necessitate additional interventions.
4. Prolonged Rehabilitation Period:
Keratoconus patients undergoing keratoplasty typically require a prolonged rehabilitation period characterized by frequent postoperative visits, suture adjustments, and visual rehabilitation exercises. This extended recovery process can affect patient satisfaction and quality of life.
5. Long-Term Medication Requirements:
Postoperative management often entails long-term use of corticosteroid eye drops or systemic immunosuppressive medications to prevent graft rejection. Prolonged medication usage may lead to systemic side effects and necessitate close monitoring by healthcare providers.

Considerations for Patient Counseling:
1. Realistic Expectations:
It is essential for keratoconus patients considering keratoplasty to have realistic expectations regarding visual outcomes. While the procedure aims to improve vision, significant visual improvement may not always be achievable due to inherent limitations.
2. Importance of Compliance:
Patient compliance with postoperative medication regimens and follow-up visits is paramount to ensure optimal graft survival and visual outcomes. Non-compliance increases the risk of complications and graft failure, compromising the effectiveness of the surgical intervention.
3. Discussion of Alternative Options:
Patients should be informed about alternative treatment modalities, including contact lenses, corneal collagen cross-linking, and newer minimally invasive techniques, which may offer viable alternatives to keratoplasty in certain cases.
Conclusion:
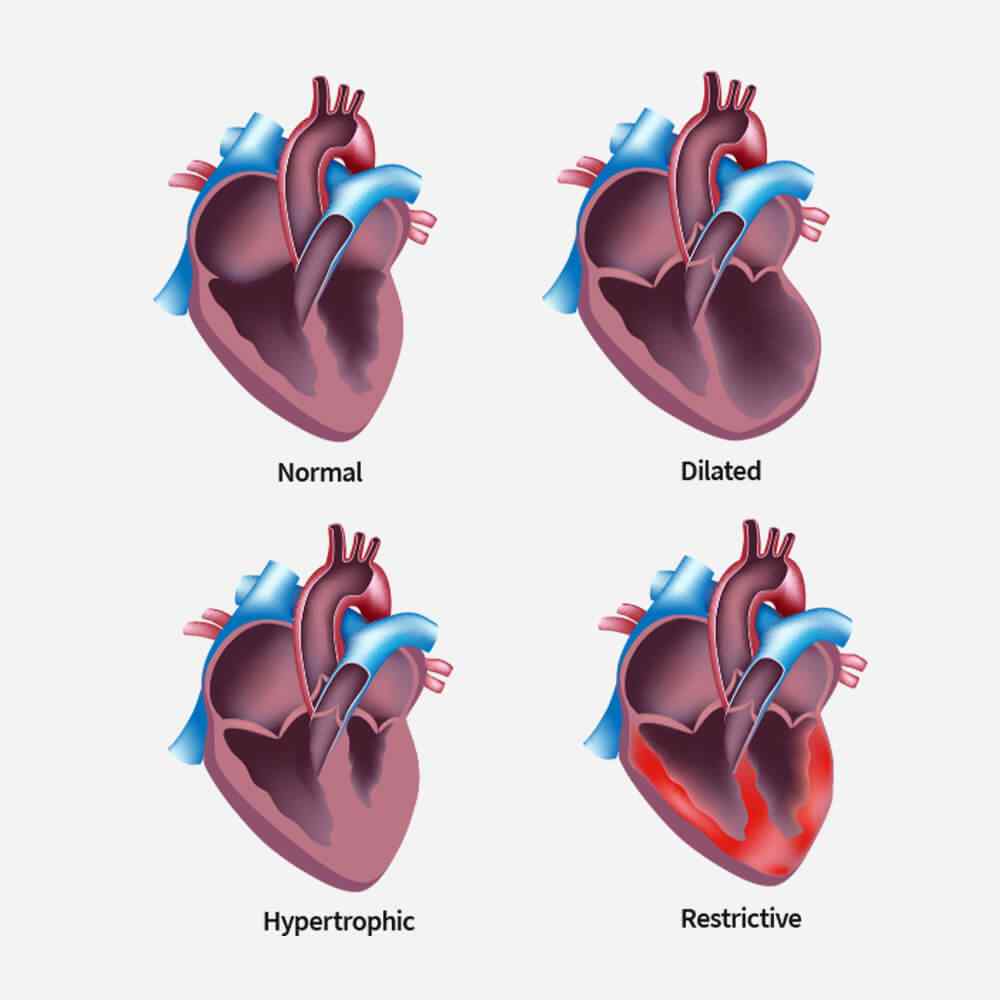
Types of Cardiomyopathy
Restrictive cardiomyopathy is a condition where your ventricles do not thicken, yet they still become stiff and rigid and cannot pump blood effectively.
In this type of cardiomyopathy, the pumping ability of your heart’s main pumping chamber — the left ventricle — becomes enlarged (dilated) and can’t effectively pump blood out of the heart.
This type involves abnormal thickening of your heart muscle, which makes it harder for the heart to work. It mostly affects the muscle of your heart’s main pumping chamber (left ventricle).
In this rare type of cardiomyopathy, the muscle in the lower right heart chamber (right ventricle) is replaced by scar tissue, which can lead to heart rhythm problems. It’s often caused by genetic mutations.
Related TreatmentAngioplasty
Angioplasty uses a tiny balloon catheter that is inserted in a blocked blood vessel to help widen it and improve blood flow to your heart. Angioplasty is often combined with the placement of a small wire mesh tube called a stent. The stent helps prop the artery open, decreasing its chance of narrowing again.