PUBLISHES ABOUT KERANATURAL
Pioneer of KeraNatural
Effect of Corneal Allogenic Intrastromal Ring Segment (CAIRS) Implantation Surgery in Patients With Keratoconus According to Prior Corneal Cross-linking Status
ABSTRACT
PURPOSE: To compare the effects of corneal allogenic intrastromal ring segment (CAIRS) implantation on topographical measurements and visual outcomes of patients with keratoconus with and without corneal cross-linking (CXL) prior to the time of implantation.
METHODS: Sixty-seven eyes with corneal allograft intrastromal ring segment implantation (KeraNatural; Lions VisionGift) due to advanced keratoconus were included in the study. Thirty-seven eyes had no CXL and 30 eyes had had CXL before being referred to the authors. The changes in spherical equivalent (SE), uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), steep keratometry (K1), flat keratometry (K2), mean keratometry (Kmean), maximum keratometry (Kmax), and thinnest pachymetry were retrospectively analyzed 6 months after the implantation.
RESULTS: The median age was 29 years in the CXL group and 24.0 years in the non-CXL group (P > .05), respectively. All topographical and visual parameters before implantation were similar in both groups (P > .05 for all parameters). At 6 months, CDVA, K1, and Kmean showed higher improvement in the non-CXL group than the CXL group (P = .030, .018, and .039, respectively).
CONCLUSIONS: CAIRS surgery has a flattening effect on both the corneas with and without CXL. The cornea with prior CXL treatment had less flattening effect due to the stiffening effect of prior CXL.
[J Refract Surg. 2024;40(6):e392-e397.]
Allograft corneal ring segment for
keratoconus management: Istanbul
nomogram clinical results
Fatma Feyza Nur Keskin, Khoa D Tran and Aylin Kilic
Abstract
Purpose: To evaluate the clinical feasibility and visual outcomes of allograft corneal ring segment implantation for the treatment of keratoconus.
Methods: This case series, included forty-four eyes of 32 patients with a 6-month follow-up. All cases were treated according to the Istanbul nomogram. In the Istanbul Nomogram, corneal tunnels of 4 × 7.5 mm diameters are created at depth of 200 μm and implanted with sterile allograft corneal rings (KeraNaturalTM, Lions VisionGift, Portland, OR, USA) at the cone location. Uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), spherical equivalent (SE) and keratometric values were compared preoperatively versus postoperatively.
Results: There was significant improvement in UDVA, CDVA, SE and topographic keratometric values. The mean pre-operative CDVA (Snellen, decimal) increased from 0.29 ± 0.20, to 0.56 ± 0.26 (P < 0.001), at the last visit. There was no statistically significant difference between preoperative and postoperative thinnest pachymetry values (P = 0.509). No major complications or adverse event were observed during and after the operation.
Conclusions: The results of this pilot study show that sterile allograft corneal ring segments may be safe, effective and enhance the visual performance of keratoconus patients. Larger clinical studies are needed to demonstrate the effective-ness and safety with long term follow-up.
Efficacy and safety of intracorneal allogenic ring segment implantation in keratoconus: 1-year results
BACKGROUND: To evaluate the safety and efficacy of corneal allogenic intrastromal ring segments in the management of keratoconus patients.
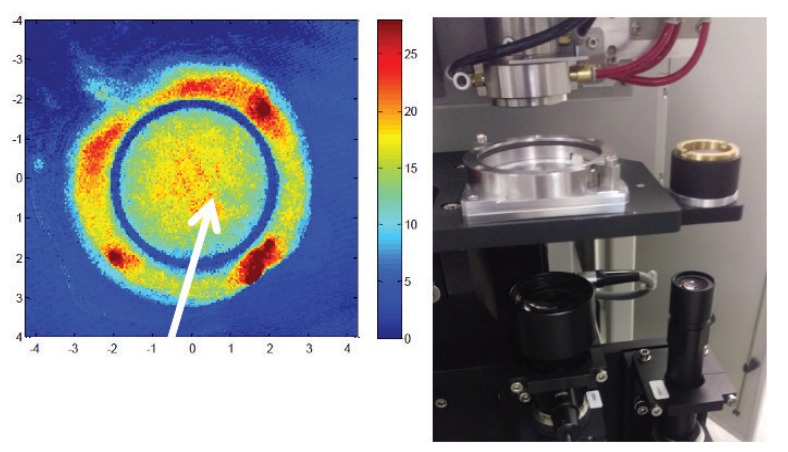
METHODS: The retrospective, nonrandomized, interventional case series consisted of 65 keratoconic eyes of 49 consecutive patients who had ring segment-shaped corneal allografts (KeraNatural®) implanted in intrastromal tunnels created using a femtosecond laser. The main outcome measures were uncorrected visual acuity (UCVA), corrected distant visual acuity (CDVA), refraction, keratometry, and pachymetry. Computed tomography scans of the corneal surfaces were also performed preoperatively as well as 3, 6 and 12 months postoperatively.
RESULTS: Mean age was 29.5 ± 7.3 years (median 29, range: 20–52 years). The mean UCVA improved from 0.91 ± 0.50 logMAR preoperatively to 0.40 ± 0.24 logMAR postoperatively at 6 month follow-up (p < 0.01) and the mean CDVA improved from 0.87 ± 0.20 logMAR preoperatively to 0.27 ± 0.06 logMAR postoperatively (p < 0.01). The mean spherical equivalent improved from −8.82 ± 4.57 to −3.45 ± 4.81D (p < 0.01). Average Keratometry decreased from 49.23 ± 5.22 preoperatively to 45.63 ± 4.89 D
postoperatively (p < 0.01). Mean anterior and posterior maximum elevation were also decreased significantly (p < 0.01). In one patient, dislocation of the graft towards the tunnel incision site and dehiscense at the tunnel entrance were observed in the firstweek of the operation. Yellow-white deposits were observed in the segment tunnels in five cases after 6 months.
CONCLUSION: This study demonstrated that implantation of corneal allograft ring segments is a viable alternative treatment for keratoconus with safety and good visual results.
Corneal Allografts for Therapeutic and Refractive Purposes
Refractive surgery provides patients with the chance to reduce or eliminate their reliance on glasses and contact lenses. LASIK, PRK, and laser-assisted lenticule extraction (LALE), however, are not universally applicable. For example, the efficacy of LASIK for the treatment of individuals with emmetropic presbyopia and young patients with more than 3.00 D of hyperopia is limited. Attempts to induce central corneal steepening can result in epithelial hyperplasia and suboptimal results. Furthermore, patients with a short axial length and shallow anterior chamber may be poor candidates for LALE. In keratoconic eyes, the inherent weakness of the cornea combined with the removal of corneal tissue during laser procedures can aggravate the condition.
Tissue addition technology is a promising alternative to treatments such as LASIK, PRK, and LALE that remove tissue. Tissue addition strengthens the corneal structure through the addition of allograft material. The technology expands the capabilities of refractive surgery by addressing challenges such as emmetropic presbyopia and pronounced hyperopia in young patients. It opens new avenues for
the treatment of keratoconus.
An Allograft or Biosyntetic Corneal Rings?
Several options are available to achieve visual rehabilitation in patients with keratoconus to avoid or delay the need for lamellar and penetrating keratoplasty. They include spectacles, contact lenses, the implantation of intrastromal corneal ring segments (ICRSs), corneal surface ablation combined with CXL, and the implantation of phakic IOLs. Now, another exciting option is on the horizon: allograft corneal rings. This article explores the potential of these technologies.
AVOIDING THE PROBLEMS ASSOCIATED WITH RING SEGMENTS
Most ICRSs currently in use are made of PMMA. These segments are implanted in the eye to induce a geometric change in the central corneal curvature, thereby improving visual acuity. One drawback to implanting these devices is that it can be associated with serious complications, including corneal melting and extrusion in eyes with thin corneas. The latter can require urgent keratoplasty and lead to permanent vision loss. Other potential complications include segment migration, endothelial perforation, corneal haze, and misdirection of the segment into deeper or more superficial layers of the cornea. Further, implanting a foreign body into the cornea may result in a loss of corneal transparency and subepithelial stromal opacity in the long term. Surgeons have turned their attention to the use of ICRSs made of allogenic corneal tissue as a potential means of improving the safety of this procedure.
The use of allogenic tissue provides biocompatibility and improved integration into the cornea and avoids problems such as inflammation related to the insertion of a synthetic material into the cornea. 3 Allogenic corneal tissue provides an unhindered passage of oxygen and nutrients to the cornea, ensuring stable corneal conditions and decreasing the risks of corneal necrosis and melt.
Lenticular Extraction And Addition
Lenticular surgery is gaining momentum, and rightfully so. More than 3.5 million SMILE procedures have been performed worldwide, and other lenticule extraction procedures are being introduced and studied. It is likely only a matter of time before these procedures are available worldwide. On top of the advances being made in lenticule extraction surgery, allogenic lenticules are now used in certain regions of the world to treat some of the hardest refractive errors to correct—emmetropic presbyopia and hyperopia—and allogenic ring segments are being studied for the treatment of keratoconus.
The future for all of these applications looks bright. The articles in this series highlight the recent advances in lenticular extraction and addition and postulate the impact of these procedures as catalysts for the growth of refractive surgery. In my guest editorial, I focus on the potential of modified epikeratophakia.
Keratoconus Management by Insertion of an Allograft Corneal Ring Segment (KeraNatural)
Hornhautringsegments
Keratoconus is a bilateral corneal ectatic disorder characterized by local biome-chanical weakness, corneal thinning, protrusion [1], asymmetrical irregular corneal astigmatism, marked anterior and posteri or elevation coinciding with the hinnest
point at pachymetry, and compensatory thinning of the corneal epithelium at the cone area [2], resulting in deterioration of vision [3].
In advanced cases with no clini-cally significant opacities or hydrops, the implantation of intracorneal ring segments for the treatment of keratoconus was first proposed by Colin et al. [4] as an alternative for selected cases and complimentary to penetrating and lamellar keratoplasty for patients with contact lens intolerance. Unfortunately, polymethyl methacrylate (PMMA) implants, although quite effective, bare a high complication rate, up to 30 % [5, 6]. The implantation of corneal allogenic intrastromal ring segments (CAIRS) was introduced by Jacob etal. [7] as a safe and effective alternative to the artificial rigid ring segments of different shapes and sizes, inducing similar flattening effects on the protruding keratoconic cornea without the possibility of serious complications like extrusion, perforation, and corneal melting often encountered by the implantation of rigid artificial implants. The aim of this report was to present the technique and results of the first implantation of a precut sterile allograft corneal ring segment (KeraNatural, VisionGift, Portland, OR, USA) in Switzerland for the management of keratoconus.
Long-Term Results of Sterile Corneal Allograft Ring Segments Implantation in Keratoconus Treatment
Purpose: To evaluate the efficacy and safety of sterile corneal allograft ring segments implantation for the treatment of keratoconus by analyzing long-term visual, refractive, and tomographic clinical outcomes.
Methods: This prospective study included 62 eyes of 49 patients with keratoconus who underwent corneal allograft ring segments implantation at Istanbul Medipol University Faculty of Medicine between February 2020 and August 2022. Surgical outcomes using the Istanbul nomogram were evaluated in patients preoperatively and postoperatively at 1 month, 6 months, 1 year, and 3 years. Outcomes measured were uncorrected distance visual acuity (UDVA), cor-
rected distance visual acuity (CDVA), spherical equivalent (SE), spherical refraction (SR), cylindrical refraction (CR), topographic keratometric values, and corneal thickness at the thinnest point.
Results: Preoperative mean UDVA and CDVA (LogMAR) were 0.96 6 0.50 and 0.72 6 0.47, respectively, and increased to 0.41 6 0.34 and 0.22 6 0.19 at the last visit (P , 0.001). There was a significant decrease in SE, SR, and keratometric values post-operatively (P , 0.001). There was no difference in CR and thinnest corneal thickness values (P = 0.333 and 0.154, respectively). The stromal and epithelial thicknesses measured by anterior segment optical coherence tomography were stabilized at 6 months and 1 year, respectively. No major complications or side effects were observed intraoperatively or postoperatively.
Conclusions: This study demonstrated that sterile corneal allograft ring segments implantation is a safe and feasible treatment for keratoconus, yielding notable long-term visual outcomes with minimal implant-related complications.
Why Dr. Aylin Kılıç
1997: Her Mentor was Prof Joseph Colin who performed first Corneal Ring in the world for KC
2003-2016: She performed more than 1000 Traditional Corneal Ring
2017: Her first corneal inlay clinical series in the world (Allotex) 130 cases, emmetropes, hypermetrops
2019: She made collaboration with USA Eye Bank (VisionGift) developed KeraNatural product and İstanbul nomogram first time in the world
2019-2024: more than 200 cases, 5 years follow-up
- 18 keranatural presentation
- 3 keranatural award
- 5 keranatural scientific academic article









